Weather Patterns Associated with Pain in Chronic-Pain Sufferers
- By David M. Schultz, Anna L. Beukenhorst, Belay Birlie Yimer, Louise Cook, Huai Leng Pisaniello, Thomas House, Carolyn Gamble, Jamie C. Sergeant, John McBeth, and William G. Dixon
- Jun 26, 2023
Hippocrates (circa 400 BCE) wrote in On Airs, Waters, and Places that diseases had seasonal cycles and the health of city dwellers was affected by prevailing wind directions. Such ideas persisted until the eighteenth century. Today, a common belief among three-quarters of patients who suffer from chronic pain is that their daily pain levels fluctuate with the weather.
Whether there is any scientific support for these beliefs remains a frustrating question to try to answer. Studies synthesizing this literature find a range of results. In a review of 43 studies examining the relationship between weather and pain in patients with chronic musculoskeletal pain, 29 (67%) found some relationship (Beukenhorst et al. 2020), although the possibility of a publication bias for positive relationships cannot be discounted.
Even among those 29 studies, however, some of the individual studies described their own results as “not clinically important” or “not clinically significant” or “making a minimal contribution to pain.” Many of these previous studies had inconclusive results because they used either relatively small sample sizes (e.g., as few as 18–25 individuals) or had surveyed patients infrequently. One study contacted participants every 3 months over a 2-yr period, yielding nine total data points per patient (Dorleijn et al. 2014).
Some studies were unable to ensure that weather observations were representative of the conditions experienced by the participants because the locations of the participants were not tracked during the study or because weather conditions were considered representative of too large an area or time. Analysis of the data also appeared to commonly lack any input from a meteorologist. This led to such issues such as assuming weather quantities could be treated as independent variables or poor choices in weather quantities or analysis approaches. Other studies seemed to selectively report results after multiple testing. Finally, most studies failed to consider other variables that might explain or otherwise affect the results, such as time spent outside or how mood or physical activity ultimately influenced pain.
The Potential Impacts of Linking Pain and Weather
If scientists could demonstrate a relationship between pain and weather, it would validate the beliefs of patients suffering from chronic pain who are often dismissed by their doctors. Also, knowing the specific weather variables involved in the weather–pain relationship could lead in the future to better understanding of how pain is created in the body, which could lead to better, more targeted approaches to treat or minimize the pain. If a weather–pain relationship existed, individualized pain forecasts derived from weather forecasts and a patient’s condition could be produced so that patients could better manage their pain and adjust their activities accordingly (e.g., by arranging reasonable adjustments with their employer to work from home when pain is expected due to weather; by avoiding outdoor labor or vigorous exercise on days when pain is expected to be enhanced due to the weather).
To overcome limitations in the design and execution of previous studies, we designed a citizen-science project called Cloudy with a Chance of Pain, funded by the United Kingdom’s leading arthritis charity Versus Arthritis. This became a U.K.-based smartphone study where participants who had chronic pain used a specially designed smartphone application (i.e., app) to enter a 10-question daily report on their level of pain, other symptoms, amount of physical activity, mood, and other questions that may affect their amount of pain. For example, participants were asked “How severe was your pain today?” and reported pain on a 5-point scale: “no pain,” “mild pain,” “moderate pain,” “severe pain,” and “very severe pain.”
Using hourly records from the global positioning system (GPS) sensor in the phone, we linked the participant’s location to the closest weather station in the Met Office observing network. Thus, we developed a daily profile of the average weather conditions each participant experienced, even accounting for their travels within the United Kingdom during the day. With geographic data collection, any increases in pain could then be related to weather (or changes in weather). And the phone app allowed us to engage a large population for a long time in a citizen-science project, to collect data as frequently as every day, and to address confounding effects that have not been addressed previously.
Cloudy with a Chance of Pain
The Cloudy with a Chance of Pain project ran for 15 months. A total of 10,584 participants from across the United Kingdom entered their demographic information and at least one pain report, making them eligible for the present study. A total of 6,850 (65%) participants remained in the study beyond their first week and 4,692 (44%) beyond their first month. Even after 200 days, 15% of participants were still entering data nearly every day. This rate of engagement is exceptionally high compared to other mobile health studies. We believe that our high retention is an indication of the easy-to-use app design, as well as the high level of interest by our participants in contributing toward an answer to this specific research question, which often has been of great personal interest to them (Druce et al. 2017, 2019).
How to define a pain event is not straightforward. The self-reported nature of the pain levels in our study could lead to bias by directly comparing one participant’s pain levels to another. For example, two persons reporting “very severe pain” (5 on our 5-point scale) may have completely different experiences. In addition, participants may use the pain scale differently (e.g., never report maximum or minimum values of pain). To avoid this dilemma, we refer to previous studies that show a 20% increase in pain is clinically significant. Such a clinically significant pain event could be measured by an increase of at least 1 category on our 5-point scale. As such, we define a pain event in an individual participant when they report a 1-category or greater increase in their pain level from the previous day (e.g., moderate pain yesterday to severe pain today). We termed this a +1 or greater pain event.
Pain events were most clearly measured among participants who entered data on two or more consecutive days. Of this group, 10%-23% reported a pain event daily. By choosing “fraction of participants with a +1 increase in pain” as our outcome, our analysis is independent of how an individual interprets the pain scale.
We also checked our results to the sensitivity of our definition of pain. We considered two other choices. The first was a 2-category or greater increase in their pain level from the previous day. Only 1% to 6% of participants reported a +2 pain event on any given day. The second was when a participant reported severe pain or very severe pain on the 5-point pain scale. This was reported by 12.7% to 26.9% of participants on any given day. Both of these choices produced similar results to those below, indicating that our results are robust to our definition of a pain event.
To study the average weather conditions on days when a high percentage of participants were reporting pain, we took the top 10% (45 days) with the largest percentage of participants having a +1 or greater pain event, termed HIGH. For comparison, we examined the bottom 10% of days with the lowest percentage of participants having a +1 or greater pain event, termed LOW. There were about twice as many participants experiencing a pain event on a HIGH day than on a LOW day.
Monthly and Weekly Pain Occurrences
The number of occurrences of the 45 HIGH days and the 45 LOW days in each calendar month were counted, then normalized by the number of days in a 30-day month. These HIGH and LOW days appear during certain months. Specifically, most HIGH days occurred in January to June 2016, whereas most LOW days occurred from June 2016 to January 2017, with a maximum in April 2017. Whether this pattern represents some sort of seasonality is uncertain, given the 15-month period of the study. But the variations in the fraction of participants experiencing a pain event by month suggests that seasonal changes in weather might be one component to understanding regulators on pain (e.g., Cutolo 2011; Park et al. 2017).
When the 45 HIGH and 45 LOW days are plotted as a function of day of the week, there is a dramatic distinction. HIGH days tend to occur throughout the week, with a slight preference for Monday and Tuesday, whereas LOW days have a much larger weekly cycle with a midweek minimum and sharp maxima on Saturday and Sunday. The analysis presented later in this article was carried out by separating LOW days into weekdays and weekend days; the results were similar for each set of days (not shown).
Surface Weather Observations
Because of the GPS in participants’ smartphones, we were able to identify the closest weather station to their location. Interestingly, each participant in the study had a median number of 9 weather stations associated with their locations during the data collection period. This indicates how mobile the participants were during the course of the study and the importance of accounting for the weather at different locations. These hourly weather observations were averaged together to construct daily weather conditions for each participant who provided reports on their pain.
The data show differences between HIGH days and LOW days for 2-m temperature, 2-m dewpoint, sea level pressure, and 10-m wind speed, with HIGH days being associated with lower temperature, lower dewpoint, lower sea level pressure, and higher wind speed. In contrast, 2-m relative humidity for HIGH and LOW pain days showed no significant difference, perhaps because the typical large diurnal cycle in relative humidity is averaged over the course of the day. The present results are also consistent with what participants believed before the study started with 6,941 (66%) saying their pain was associated with cold and with 3,687 (35%) saying their pain was associated with changes in barometric pressure. Additionally, 83 participants said their pain was associated with “wind” and 49 participants said their pain was associated with “storm” (i.e., low pressure), again supportive of these results.
Refining the Weather Analysis with Synoptic Composites
Synoptic compositing is a common technique in synoptic meteorology. It consists of taking the mean of a number of weather maps that have some event in common. Composite analyses are constructed from the NOAA/ESRL website using the NCEP–NCAR reanalysis (Kalnay et al. 1996). The 1200 UTC weather maps for each day we averaged together to produce the composites. To examine fields in the lower troposphere, we selected 925 hPa (about 750–800 m above sea level). Other levels in the lower troposphere were also investigated (i.e., surface, 850 hPa) for the quantities described below and yielded similar results.
Composite analysis of 500-hPa geopotential height, sea level pressure, precipitation, 925-hPa moisture, wind, and temperature reveal the weather patterns present during HIGH versus LOW days. Anomalies are computed from averages of the daily-mean fields. During HIGH days, a trough lay over the United Kingdom, North Sea, and Norway, indicated by a −40-m 500-hPa height anomaly and a −5-hPa sea level pressure anomaly. This surface pressure anomaly associated with a 500-hPa height anomaly indicates the tropospheric-deep structure of the flow on HIGH days. Also, a ridge lay to the southwest over the North Atlantic Ocean. During LOW days, on the other hand, a ridge lay over the United Kingdom, indicated by a +60-m 500-hPa height anomaly and a +5-hPa sea level pressure anomaly, with anomalously low heights southeast of Greenland. The difference between the patterns on HIGH and LOW days indicates remarkably different weather patterns for the United Kingdom.
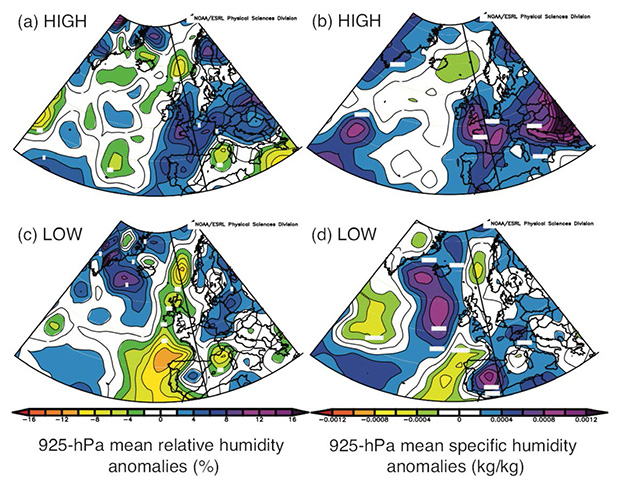
Synoptic composites of (a),(b) HIGH and (c),(d) LOW days. (a),(c) 925-hPa mean relative-humidity anomalies [colored according to the scale in (c)]. (b),(d) 925-hPa mean specific-humidity anomalies [colored according to the scale in (d)]. Anomalies computed relative to the weighted average of the daily 1981–2010 means. Images provided by the NOAA / ESRL Physical Sciences Division, Boulder, Colorado, from their website
The 925-hPa relative humidity and specific humidity on HIGH days shows a band of more humid air extending from Spain to the United Kingdom and a local maximum in daily average precipitation rate over the United Kingdom. In contrast, the same fields on LOW days show a dry anomaly over the same band and a similarly shaped region of minimum precipitation rate.
In line with the height field in HIGH, the 925-hPa mean wind field shows the United Kingdom in the left-exit region of westerly flow. In contrast, the wind field in LOW shows the jet moving north of the United Kingdom, consistent with the ridge. The values of mean winds from the reanalyses over the United Kingdom are roughly the same on HIGH and LOW days. 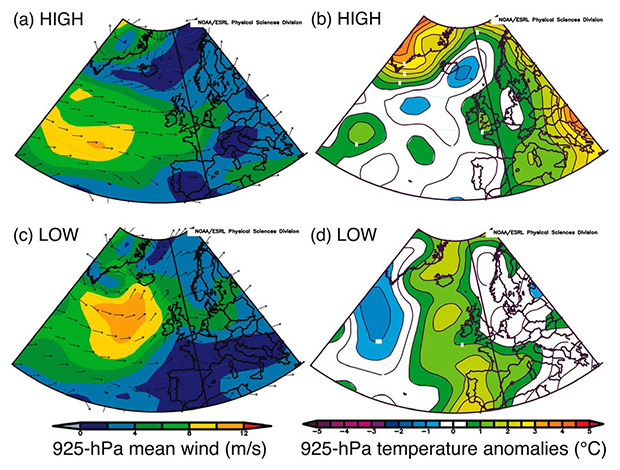
Synoptic composites of (a),(b) HIGH and (c),(d) LOW days. (a),(c) 925-hPa mean wind speed [colored according to the scale in (c)] and direction (arrows). (b),(d) 925-hPa temperature anomalies relative to the weighted average of the daily 1981–2010 means [colored according to the scale in (d)]. Images provided by the NOAA / ESRL Physical Sciences Division, Boulder, Colorado, from their website
The 925-hPa temperature anomalies on HIGH days show warmer air over and east of the United Kingdom, with cooler air to the west. In contrast, the temperature on LOW days is also anomalously high over the United Kingdom and to the west, but the anomaly is less than for HIGH. These results suggest that HIGH days (when a high percentage of participants experience a pain event) occur with lower pressure over the United Kingdom, which is also associated with more wind, moisture, and precipitation. In contrast, on LOW days (when a low percentage of participants experience a pain event) higher pressure over the United Kingdom brings weaker winds and drier air.
More Studies Needed
Although the results are intriguing, these findings from the United Kingdom should not necessarily be extrapolated to different climates where the weather is different. Such a study as Cloudy with a Chance of Pain should be replicated elsewhere to determine if the weather patterns associated with painful days presented here generalize to other locations in other climates.
Another caveat with this study is that the analysis involved all 10,584 who participated and suffered from chronic pain (i.e., a population-wide analysis). Participants were living with one or more of a number of different diseases such as unspecified arthritis (34.6%), fibromyalgia or other widespread pain (26.4%), osteoarthritis (24.1%), rheumatoid arthritis (18.5%), neuropathic pain (15.1%), chronic headache and migraine (10.3%), and gout (3.5%). The present analysis assumes that all participants would have the same weather–pain relationship. Different diseases may have different sensitivities to pain, and—even within and across diseases—participants may be affected differently due to pathology, genetics, or other factors. For example, someone with constant severe pain may not be affected by, or may not notice, fluctuations caused by the weather. Using the whole population means that our results may underestimate the most important associations for subsets of our population. Initial analyses revealed no notable differences when stratifying the results by pain condition, although the smaller sample sizes limited statistical power. Work on identifying subsets of our population continues.
A third caveat is that the amount of time spent inside by participants will affect their exposure to the weather. Because the air pressure inside a building is generally in equilibrium with the air pressure outside, that should not be a factor. However, the temperature and humidity of air inside the building often differs from that outside, and being inside is protection from wind and precipitation. So, if the weather affects people’s pain, we might expect to see some influence from the amount of time spent outside. However, the relationship between weather, pain, and time spent outside is complex; time spent outside is often influenced by an individual’s pain, meaning we might expect different levels of pain in participants who are indoors versus outdoors, irrespective of the weather. Untangling the effect of those who stayed inside because their pain was severe and those who were inside for other reasons is difficult and requires further analysis.
Conclusions
Some small inconsistencies exist, but the results are consistent with lower pressure over the United Kingdom associated with more wind, moisture, and precipitation on HIGH days when a high percentage of participants experience a pain event. In contrast, on LOW days when a low percentage of participants experience a pain event, higher pressure over the United Kingdom brings weaker winds and drier air.
On any given day, about 16% of people suffering with chronic pain experienced a +1 or greater pain event in the United Kingdom, a number that increased to a maximum of 23% on a high-pain day and decreased to a minimum of 10% on a low-pain day. Weather patterns can explain a portion of that variability. Although the weather may not be the primary cause of people’s pain, our results through multiple independent methodologies demonstrate that weather does modulate pain in at least some individuals. Who is the most susceptible remains to be determined with our dataset in the future.
The results of this project should give comfort and support to those who have claimed that the weather affects their pain, but have been dismissed by their friends, their coworkers, and even their doctors. Finally, our research also begins to shed light on the environmental conditions that modulate pain, insight that might be explored further for improving the treatment, management, and forecasting of pain.